Abstract
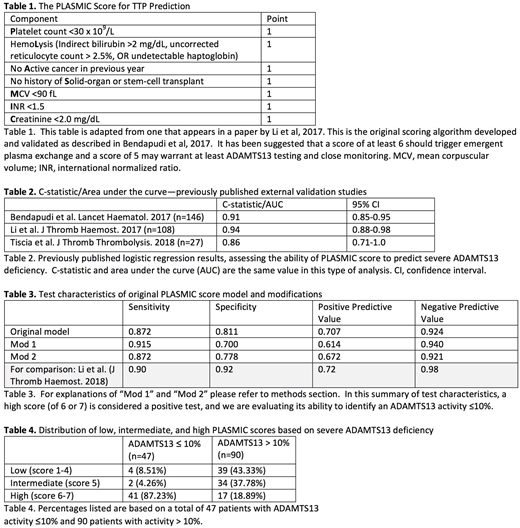
Background: Bendapudi et al. (Lancet Hematol. 2017) have recently developed and validated a clinical scoring system, the "PLASMIC score," to aid in assessing the risk of thrombotic thrombocytopenic purpura (TTP) in the absence of ADAMTS13 activity (Table 1). Although a few external validations describe good to excellent discriminatory value (Table 2), our experience using the PLASMIC score has not been helpful overall. We sought to perform our own validation of the PLASMIC score for clinical prediction of severe ADAMTS13 deficiency.
Methods: We evaluated 323 patients who had ADAMTS13 testing performed between January 1, 2006 and June 20, 2018. We excluded patients who did not meet criteria for thrombotic microangiopathy (TMA), defined as schistocytes noted on peripheral blood smear within 2 days prior to ADAMTS13 testing and platelet count ≤ 100 x 109/L on the day of ADAMTS13 testing. We also excluded patients who were seen as outpatients, had PLEX elsewhere prior to admission, presented with a known TTP history, had possible interferences with the ADAMTS13 assay, or had irretrievable records. A total of 186 patients were excluded, including 9 "missing data" patients for whom all 7 components of the PLASMIC score were not available to calculate a score. 137 patients were included in the final analysis, 90 with an initial ADAMTS13 activity >10% and 47 with a severe deficiency (≤10% activity). We calculated a PLASMIC score for each patient, using the earliest admission laboratory values if initial ADAMTS13 testing was within Day 3 of admission. If initial ADAMTS13 testing occurred on or after Day 4 of admission, we used the closest laboratory values within 5 days prior to ADAMTS13 testing. This methodology was used in previous external validations of the PLASMIC score. We also experimented with two modifications on the original methodology. Our first modified PLASMIC score ("Mod 1") was designed to maximize the PLASMIC score, in order to err on the side of caution and help avoid missing potential TTP. Rather than just the earliest or closest laboratory value, any eligible laboratory value within 5 days prior to ADAMTS13 testing could be used to assign 1 point for a given category. Our second modified score ("Mod 2") assigns 1 point for serum creatinine <2.5 mg/dL rather than <2.0 mg/dL. With <7% of patients with missing data, we were able to use complete-case analysis for logistic regression.
Results: The original PLASMIC score model predicted severe ADAMTS13 deficiency with a concordance "c" statistic of 0.88, where a value of 1 would indicate perfect prediction. The Mod 1 and Mod 2 models had a c statistic of 0.87 and 0.88, respectively. Sensitivity, specificity, and positive and negative predictive value for each of these 3 models, when PLASMIC score was dichotomized at high (score 6-7) versus low-intermediate risk (score ≤ 5), are summarized in Table 3. Almost 20% of patients with ADAMTS13 activity >10% had high scores, and the majority had a score of intermediate (score = 5) or higher (Table 4). We performed chi-square testing for each original PLASMIC score parameter; there was no statistically significant relationship between presence of severe ADAMTS13 deficiency and mean corpuscular volume <90 fL (z-score, p = 0.236). Among those patients with a high risk PLASMIC score by original methodology, we found a significant improvement in overall survival for those patients who received PLEX versus those who did not (log rank, p =0.0003), while no such difference was found among those with a low-intermediate risk score (log rank, p =0.3085).
Conclusion: Our study uses a sample size similar to previously published external validations and shows a lower predictive value (c = 0.88) of the PLASMIC score for identifying a severe ADAMTS13 deficiency. Across all 3 of our models the specificity is also lower than previously published (81%, vs. 92%). Our first modification increased sensitivity while decreasing specificity compared to the original model, while the second modification had results similar to the original model. Overall our results suggest that the PLASMIC score may not show the same diagnostic performance across all populations and may cause an increase in unnecessary PLEX.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal